Attorney-Verified Do Not Resuscitate Order Document for New York State
Common mistakes
-
Failing to include the patient's full name. It is essential to provide the complete legal name to avoid any confusion.
-
Not having the form signed by a physician. A physician's signature is necessary for the order to be valid.
-
Leaving the date of the order blank. The date helps establish when the directive was created.
-
Not discussing the order with family members. Open communication can prevent misunderstandings later.
-
Using outdated forms. Always ensure that you are using the most current version of the Do Not Resuscitate Order form.
-
Failing to provide clear instructions about the patient's wishes. The form should clearly reflect the patient's preferences.
-
Not keeping copies of the completed form. It’s important to have copies accessible to family and healthcare providers.
-
Neglecting to review the order periodically. Changes in health status may require updates to the order.
Learn More on This Form
-
What is a Do Not Resuscitate (DNR) Order in New York?
A Do Not Resuscitate Order is a legal document that allows a person to refuse resuscitation in the event of cardiac arrest or respiratory failure. In New York, this order instructs medical personnel not to perform CPR or other life-saving measures if the individual’s heart stops or they stop breathing.
-
Who can request a DNR Order?
In New York, a DNR Order can be requested by a patient who is at least 18 years old and has the capacity to make their own medical decisions. If the patient is unable to make decisions, a legally authorized representative, such as a healthcare proxy or a family member, may initiate the process.
-
How do I obtain a DNR Order form?
You can obtain a DNR Order form from your healthcare provider, hospital, or the New York State Department of Health website. It is important to ensure that the form is filled out correctly and signed by the appropriate parties.
-
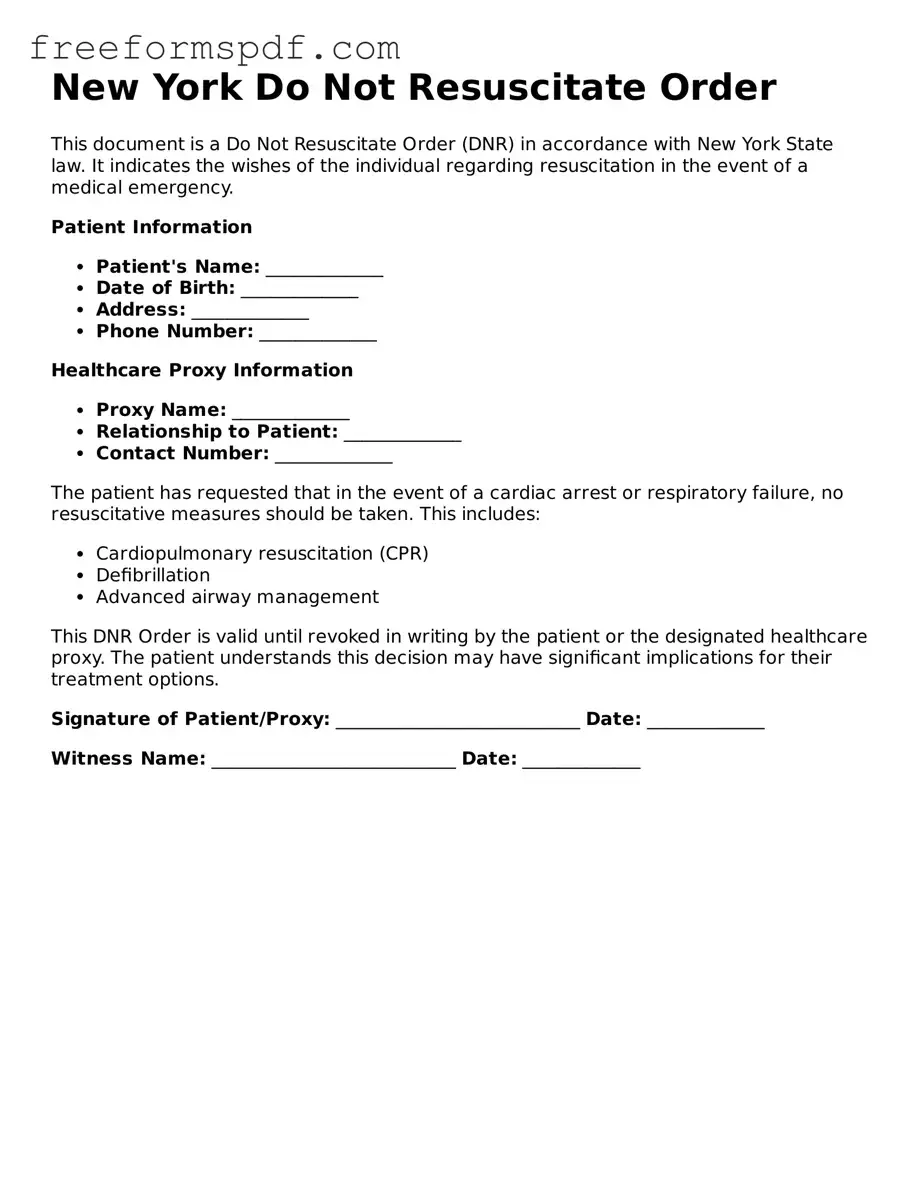
What information is required on the DNR Order form?
The DNR Order form typically requires the patient's name, date of birth, and a statement of their wishes regarding resuscitation. It must be signed by the patient or their authorized representative and a physician. The physician’s signature confirms that the patient has been informed about the order and its implications.
-
Where should I keep my DNR Order?
It is crucial to keep the DNR Order in a place that is easily accessible to emergency medical personnel. Many people choose to keep a copy in their medical records, with their healthcare proxy, or on their refrigerator. Additionally, wearing a medical alert bracelet or necklace can help ensure that first responders are aware of the order.
-
Can I change or revoke my DNR Order?
Yes, you can change or revoke your DNR Order at any time. To do this, simply complete a new DNR Order form and ensure that it is signed and dated. Inform your healthcare provider and family members about the change to avoid confusion in an emergency situation.
-
What happens if I do not have a DNR Order?
If you do not have a DNR Order in place, medical personnel are required to attempt resuscitation if your heart stops or you stop breathing. This is true even if you have expressed a desire not to be resuscitated verbally. Having a DNR Order ensures that your wishes are respected in such critical situations.
Misconceptions
Understanding the New York Do Not Resuscitate (DNR) Order form can be challenging, and several misconceptions often arise. Here are nine common misunderstandings, along with clarifications to help you navigate this important topic.
- A DNR order means no medical treatment at all. Many people mistakenly believe that a DNR order prevents all forms of medical intervention. In reality, a DNR order specifically pertains to resuscitation efforts, such as CPR or defibrillation, but does not limit other treatments or care.
- Only terminally ill patients can have a DNR order. While DNR orders are frequently associated with terminal illnesses, anyone can request one. The order is applicable to individuals who wish to avoid resuscitation in the event of cardiac arrest, regardless of their overall health status.
- A DNR order is permanent and cannot be changed. This is not true. A DNR order can be revoked or modified at any time. Patients or their healthcare proxies can communicate their wishes to healthcare providers, ensuring that the order reflects their current preferences.
- Healthcare providers will ignore a DNR order if they believe it is not in the patient's best interest. Healthcare professionals are legally obligated to respect a valid DNR order. Ignoring it would violate the patient's rights and ethical standards in medical practice.
- A DNR order only applies in hospitals. This misconception overlooks the fact that a DNR order is valid in various settings, including homes, nursing facilities, and other healthcare environments. It is crucial for patients to ensure that their wishes are communicated clearly in any setting.
- Family members can override a DNR order. Generally, family members do not have the authority to override a DNR order that has been legally established. Only the patient or their legally designated healthcare proxy can make changes to the order.
- You need a lawyer to complete a DNR order. While legal advice can be beneficial, it is not necessary to have a lawyer to fill out a DNR order. The form is designed to be accessible, and individuals can complete it with guidance from healthcare providers.
- A DNR order is the same as an advance directive. Although both documents relate to medical care preferences, they serve different purposes. An advance directive encompasses a broader range of healthcare decisions, while a DNR specifically addresses resuscitation efforts.
- Once a DNR order is signed, it is automatically recognized everywhere. This is a common misconception. It is essential to ensure that the DNR order is properly documented and communicated to all relevant parties, including healthcare providers and emergency personnel, to ensure it is honored.
By understanding these misconceptions, individuals can make informed decisions regarding their healthcare preferences and ensure that their wishes are respected in critical situations.
Some Other Do Not Resuscitate Order State Templates
How Old Do You Have to Be to Sign a Dnr - It is essential to inform your healthcare proxies about your DNR wishes.
To assist parents in understanding their obligations, the necessary Homeschool Letter of Intent guidelines provide crucial insight into the steps for filing this important document.
Dnr Directive - The DNR order must comply with state laws to be valid and enforceable in emergencies.
Dnr and Dni Documents Are All Part of What Are Known as - A DNR Order is essential for clear communication about medical wishes.