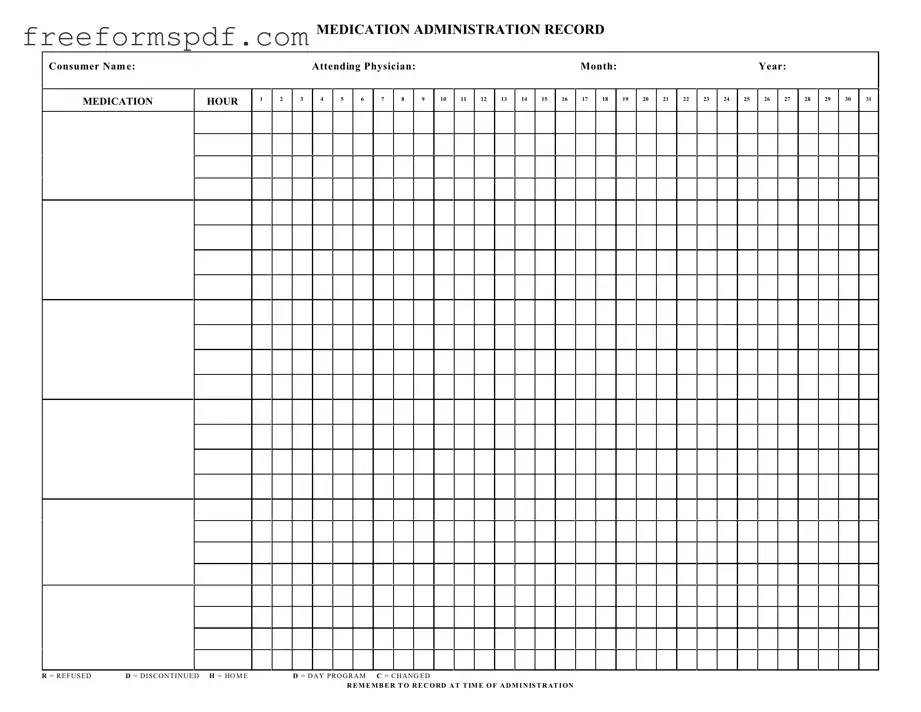
Fill in a Valid Medication Administration Record Sheet Template
Common mistakes
-
Incomplete Information: Failing to fill in all required fields, such as the consumer's name, attending physician, or date, can lead to confusion and potential errors in medication administration.
-
Incorrect Time Entries: Not recording the exact time when medication is administered can result in missed doses or double dosing. It is essential to document the administration time accurately.
-
Misunderstanding Abbreviations: Misinterpreting the abbreviations used on the form, such as R for refused or D for discontinued, may cause significant issues in medication management.
-
Neglecting to Update Changes: Failing to note any changes in medication, such as dosage adjustments or new prescriptions, can lead to administering outdated or incorrect medications.
Learn More on This Form
-
What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet is used to track the administration of medications to consumers. It helps ensure that medications are given at the correct times and allows for accurate record-keeping of any refusals or changes in medication.
-
How should I fill out the Medication Administration Record Sheet?
Begin by entering the consumer's name, the attending physician's name, and the month and year at the top of the form. Then, for each medication hour, mark the appropriate box to indicate whether the medication was administered, refused, or discontinued. Be sure to record any changes or notes as needed.
-
What do the abbreviations R, D, H, M, and C mean?
These abbreviations stand for the following:
- R = Refused
- D = Discontinued
- H = Home
- M = Day Program
- C = Changed
Use these codes to document any changes in medication administration status.
-
Why is it important to record medication administration at the time it is given?
Recording medication administration at the time it is given ensures accuracy and helps prevent errors. It allows for real-time tracking of medication compliance and provides a reliable record for healthcare providers to review.
-
What should I do if a consumer refuses their medication?
If a consumer refuses their medication, mark the appropriate box with an "R" on the record sheet. It is also important to document the reason for the refusal if known and report it to the attending physician or relevant staff for further action.
-
Can I make changes to the Medication Administration Record Sheet after it has been filled out?
Changes should be made with caution. If a correction is necessary, it is best to draw a single line through the incorrect entry, initial it, and then write the correct information. This maintains the integrity of the record while providing clarity.
-
How long should the Medication Administration Record Sheet be kept?
The record should be kept for a specified duration as determined by your organization’s policy, often for several years. This ensures that there is a comprehensive record of medication administration for auditing and legal purposes.
-
Who is responsible for ensuring the Medication Administration Record Sheet is completed accurately?
The responsibility lies with the staff administering the medication. It is crucial that all personnel involved in medication administration are trained and understand the importance of accurate record-keeping.
Misconceptions
Understanding the Medication Administration Record Sheet (MARS) is crucial for ensuring proper medication management. However, several misconceptions can lead to confusion. Here are six common misunderstandings about this important document:
- Misconception 1: The MARS is only for nurses.
- Misconception 2: The MARS is optional.
- Misconception 3: Any error on the MARS can be easily corrected later.
- Misconception 4: The MARS only tracks medication administration times.
- Misconception 5: Once medications are recorded, they do not need to be reviewed.
- Misconception 6: The MARS is only relevant during hospital stays.
While nurses often complete the MARS, it is a tool used by all healthcare providers involved in a patient's care. This includes doctors, pharmacists, and even caregivers in certain settings.
The MARS is a required document in many healthcare settings. It helps ensure that medications are administered safely and effectively, providing a legal record of what has been given to the patient.
While corrections can be made, it is important to document them properly. Errors should be noted with a clear explanation to maintain the integrity of the record.
In addition to administration times, the MARS records refusals, discontinued medications, and changes in medication. This comprehensive tracking is vital for patient safety and care continuity.
Regular reviews of the MARS are essential. They help identify any discrepancies or issues that may arise, ensuring that the medication regimen remains appropriate for the patient’s needs.
The MARS is also used in outpatient settings, long-term care facilities, and home health care. It is a critical document for any situation where medication is administered.
By addressing these misconceptions, healthcare providers can enhance their understanding and use of the Medication Administration Record Sheet, ultimately improving patient care and safety.
Browse More Forms
Navpers 1336 3 - Travel mode options are provided for the applicant's convenience when planning leave.
To navigate the complexities of property rentals in Arizona, it is crucial to utilize a reliable resource for your Arizona Lease Agreement form essentials. This document not only defines the relationship between landlord and tenant but also serves as a safeguard for both parties throughout the rental term.
Fake Doctors Note for Work - Utilize this form to communicate directly from your healthcare provider.