Do Not Resuscitate Order Document
Do Not Resuscitate Order - Customized for Each State
Common mistakes
-
Not discussing the decision with family members. Communication is essential to ensure everyone understands the wishes expressed in the DNR order.
-
Failing to provide a clear signature. A missing or unclear signature can render the document invalid.
-
Using outdated forms. Always ensure you have the most current version of the DNR order form as regulations may change.
-
Neglecting to specify the patient's name. Omitting this crucial detail can lead to confusion about whose wishes are being documented.
-
Not including the date of completion. This information is vital for understanding the timing of the decision.
-
Overlooking the need for a witness signature. Many states require a witness to validate the order.
-
Failing to consult with a healthcare professional. It's important to understand the implications of a DNR order before filling it out.
-
Not keeping copies of the completed form. Always retain a copy for personal records and provide one to your healthcare provider.
-
Assuming the form is permanent. DNR orders can be revoked or modified; it’s essential to review them regularly.
-
Ignoring state-specific requirements. Each state may have unique rules regarding DNR orders that must be followed.
Learn More on This Form
-
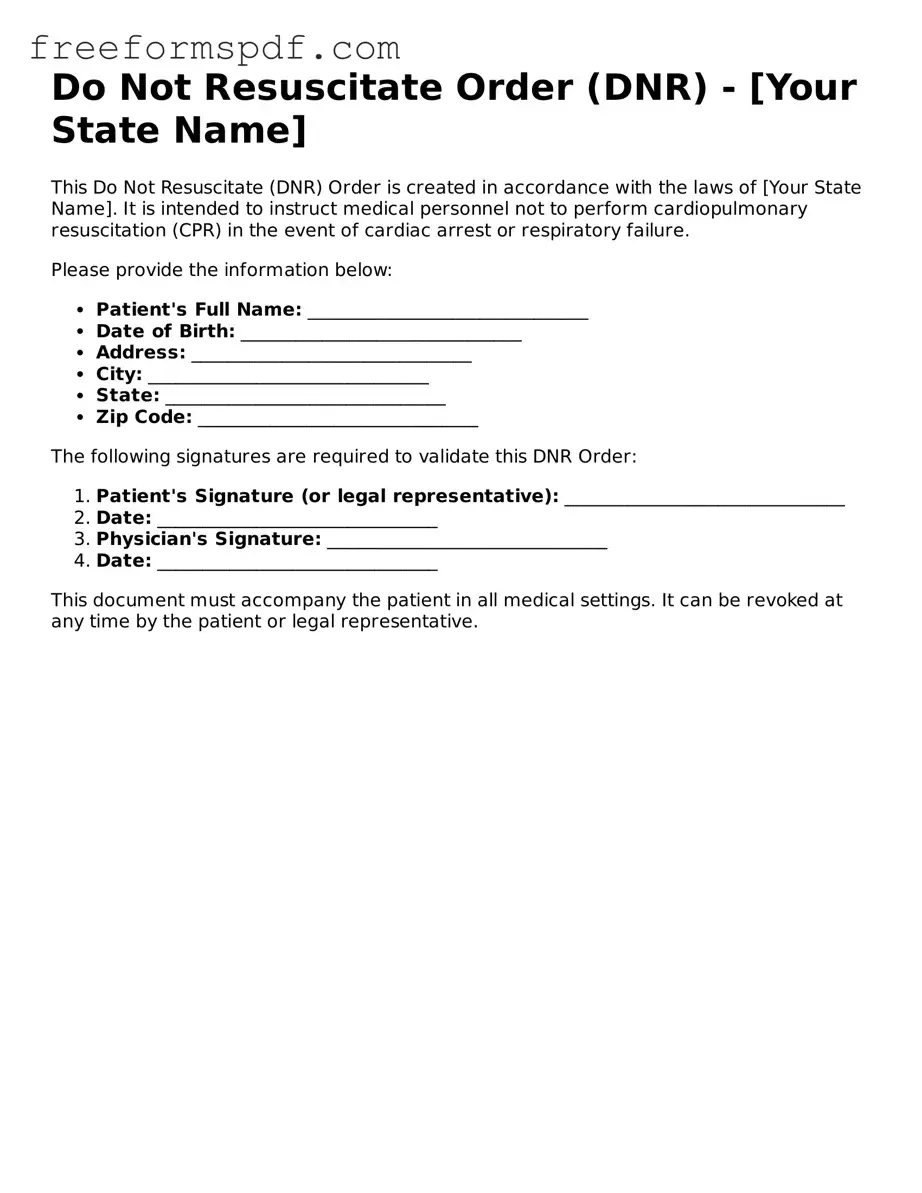
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that tells medical staff not to perform CPR or other life-saving measures if a person's heart stops or they stop breathing. It’s a way for individuals to express their wishes regarding end-of-life care.
-
Who can create a DNR Order?
Typically, adults who are mentally competent can create a DNR Order. In some cases, a legal guardian or healthcare proxy can make this decision for someone who is unable to do so.
-
How do I obtain a DNR Order?
You can usually obtain a DNR Order through your healthcare provider. They will provide you with the necessary form and guide you through the process. It’s important to discuss your wishes with your doctor before completing the form.
-
Is a DNR Order the same as an advance directive?
No, a DNR Order is a specific type of advance directive. While a DNR focuses solely on resuscitation efforts, an advance directive can include a broader range of healthcare decisions, such as preferences for other types of medical treatment.
-
Where should I keep my DNR Order?
Keep your DNR Order in a place that is easily accessible. It’s a good idea to have copies at home, in your medical records, and with your healthcare proxy. Inform your family and friends about its location, so they can provide it to medical personnel if needed.
-
Can I change or revoke my DNR Order?
Yes, you can change or revoke your DNR Order at any time. To do this, you should complete a new form and notify your healthcare provider and family members about the change.
-
Will a DNR Order affect other medical treatments?
A DNR Order specifically addresses resuscitation efforts. It does not prevent you from receiving other medical treatments. You will still receive necessary care for your condition, except for resuscitation measures.
-
What happens if I am hospitalized and have a DNR Order?
If you are hospitalized and have a DNR Order, the medical team will respect your wishes. They will not perform CPR if your heart stops or if you stop breathing, but they will continue to provide other forms of treatment as needed.
-
How can I ensure my DNR Order is honored?
To ensure your DNR Order is honored, communicate your wishes clearly with your healthcare provider and family. Make sure they understand your preferences. Additionally, wear a medical alert bracelet or carry a card that indicates you have a DNR Order.
Misconceptions
Many people have misunderstandings about Do Not Resuscitate (DNR) Orders. These misconceptions can lead to confusion and distress during critical moments. Here are nine common misconceptions about DNR Orders:
- DNR means no medical care at all. Many believe that a DNR order means a patient will receive no medical treatment. In reality, a DNR only applies to resuscitation efforts, such as CPR. Other medical treatments can still be provided.
- DNR orders are only for terminal patients. Some think that only patients with terminal illnesses can have a DNR. However, anyone can request a DNR order, regardless of their health status.
- A DNR order is permanent. People often assume that once a DNR is in place, it cannot be changed. In fact, patients or their healthcare proxies can revoke or modify a DNR order at any time.
- DNR orders are the same in every state. Many believe that DNR orders have a universal meaning. Each state has its own laws and regulations regarding DNR orders, which can affect how they are implemented.
- Doctors can impose a DNR order without consent. Some think that healthcare providers can decide to place a DNR order without discussing it with the patient or their family. In most cases, consent is required from the patient or their legal representative.
- A DNR order means giving up hope. Many view a DNR as a sign of despair. In reality, it can be a thoughtful decision that respects a person's wishes about end-of-life care.
- All healthcare facilities accept DNR orders. Some believe that every hospital or care facility will honor a DNR order. It's important to confirm that a facility recognizes and follows DNR orders, as policies can vary.
- A DNR order is only relevant in a hospital. Some think DNR orders only apply in hospital settings. However, they can also be relevant in home care or long-term care facilities.
- Having a DNR order means you will die sooner. Many fear that having a DNR order will lead to premature death. However, research shows that having a DNR does not impact overall mortality rates; it simply reflects a patient's wishes regarding resuscitation.
Understanding these misconceptions can help individuals make informed decisions about their healthcare preferences and ensure their wishes are respected.
Popular Forms:
Netspend Dispute Email - Your signature is required to validate the dispute notification.
The NYCERS F170 form plays a vital role for certain members of NYCERS who are navigating their retirement options, including the opportunity to explore resources like NY Templates for guidance in completing the necessary paperwork. This form specifically aids Tier 1 and Tier 4 members in participating in the Optional 25-Year Retirement Program for Emergency Medical Technicians (EMT), while Tier 2 members may consider the Optional 25-Year Improved Retirement Program instead.
Cease and Desist Trespassing Letter Template - This letter serves as a formal notice of no trespassing on my property.