Fill in a Valid Annual Physical Examination Template
Common mistakes
-
Incomplete Personal Information: Many individuals forget to fill in all required fields, such as their name, date of birth, or address. This can lead to delays or the need for additional appointments.
-
Missing Medical History: Some people overlook the section for diagnoses and significant health conditions. Providing a complete medical history is crucial for accurate assessment.
-
Omitting Current Medications: It’s common to forget to list all medications, including over-the-counter drugs and supplements. This information helps healthcare providers avoid potential drug interactions.
-
Neglecting Allergies: Failing to mention allergies or sensitivities can lead to serious health risks. Always include any known allergies to medications or other substances.
-
Not Updating Immunization Records: Some individuals may not provide the most recent dates of immunizations. Keeping this information current is essential for preventive care.
-
Forgetting to Indicate Health Changes: Changes in health status from the previous year should be clearly noted. This information can significantly impact the examination and recommendations.
-
Skipping Evaluation of Systems: It's easy to overlook the evaluation of systems section. This part is important for identifying any potential health issues that may not be immediately obvious.
-
Ignoring Additional Comments: Some may neglect to provide extra comments or recommendations for health maintenance. This space is valuable for conveying important information to the healthcare provider.
Learn More on This Form
-
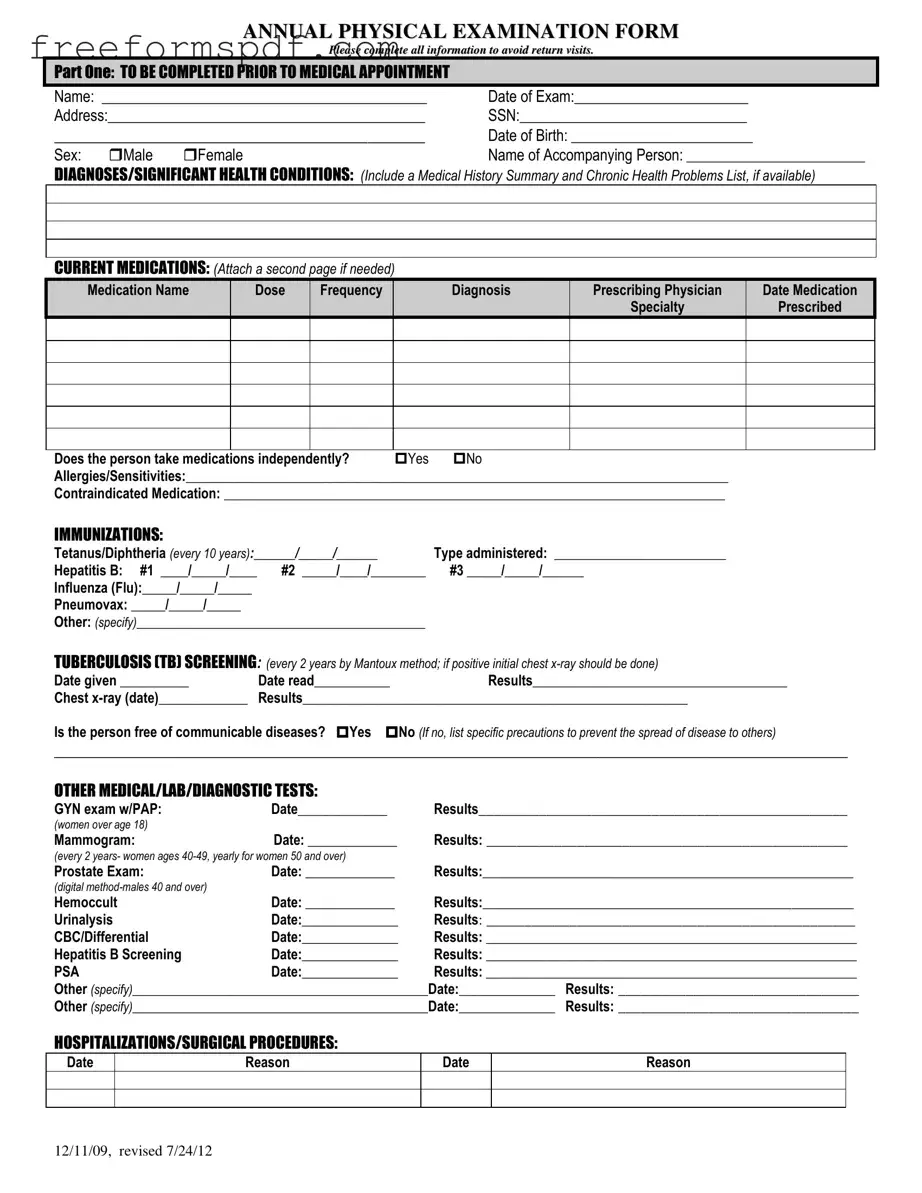
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect important health information prior to a medical appointment. This information helps healthcare providers assess a patient's overall health, manage existing conditions, and identify any new health issues.
-
What information is required in Part One of the form?
Part One requires personal details such as the patient's name, date of exam, address, social security number, date of birth, sex, and the name of an accompanying person. Additionally, it asks for a summary of diagnoses, current medications, allergies, immunization history, and tuberculosis screening results.
-
How should current medications be documented?
Current medications should be listed by name, dose, frequency, diagnosis, prescribing physician, and the date prescribed. If more space is needed, an additional page can be attached. It is also important to indicate whether the individual takes medications independently.
-
What immunizations need to be recorded?
The form requires documentation of several immunizations, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax. Dates of administration and type of vaccine administered should be noted. Additional immunizations can also be specified if applicable.
-
What tests are included in the medical evaluation?
The evaluation includes a variety of tests such as GYN exams with PAP smears for women, mammograms, prostate exams for men, and other lab tests like urinalysis and CBC/Differential. Dates and results of these tests should be documented on the form.
-
What should be done if there are allergies or sensitivities?
If the individual has allergies or sensitivities, this information must be clearly stated on the form. It is crucial for healthcare providers to know about any contraindicated medications to avoid adverse reactions.
-
How is the physical examination section completed?
The physical examination section includes vital signs such as blood pressure, pulse, respiration, temperature, height, and weight. Additionally, the evaluation of various systems (e.g., eyes, ears, cardiovascular) requires a simple "yes" or "no" response, along with comments if necessary.
-
What are the recommendations for health maintenance?
Recommendations for health maintenance should include suggestions for lab work, treatments, therapies, exercise, hygiene, and weight control. These recommendations help ensure ongoing health and wellness for the individual.
-
What happens if there are changes in health status?
If there has been a change in health status from the previous year, it should be specified on the form. This information is essential for healthcare providers to understand the patient's current condition and adjust care plans accordingly.
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion and missed opportunities for health management. Here are some common misunderstandings:
- It's only for sick people. Many believe the exam is only necessary when feeling unwell. In reality, regular check-ups help prevent health issues.
- All information is optional. Some think they can skip sections. Completing all fields is crucial for accurate assessments.
- Immunizations are not important. Some individuals underestimate the value of vaccines. Staying updated on immunizations is essential for long-term health.
- Only doctors need to fill it out. This form requires input from patients too. Your medical history and current medications are vital for effective care.
- It’s the same every year. Each year’s form may differ based on your health changes. Regular updates are necessary for accurate evaluations.
- Past health issues are irrelevant. Many think previous conditions don't matter anymore. However, they can significantly impact current health assessments.
- Results are always immediate. Some expect instant feedback. Lab results and other evaluations may take time, and follow-up is often necessary.
- Physical exams are just a formality. Many view them as unnecessary. In truth, they are a critical component of preventive health care.
Browse More Forms
Prescription Slip - Improves communication between healthcare providers and pharmacies.
For those seeking to navigate the complexities of tax benefits in New York, understanding the New York DTF-84 form is vital. This form serves as an application for Qualified Empire Zone Enterprise (QEZE) Sales Tax Certification and is particularly crucial for businesses recognized by Empire State Development. To streamline the process, applicants may find valuable resources at NY Templates, helping ensure that all necessary documentation is properly submitted to access the available tax benefits.
Osha 301 Requirements - Fosters a culture of safety by encouraging reporting of all incidents.